HOSPITAL PROCEDURES
Surgery is an invasive medical intervention using incisions to allow a healthcare provider to structurally change the body to treat or diagnose an illness or condition. The term "surgical procedure" is often used, which can be confusing. When healthcare providers use this term, it is referring to surgery.
Surgical procedures cover a vast array of interventions, ranging from minor outpatient procedures to complex surgeries requiring specialized teams and equipment. The specific procedure performed depends on the patient's medical condition, the goals of treatment, and the expertise of the surgical team.
EXPLORE YOUR HOSPITAL SURGERIES WITH CSRH!
CONE BIOPSY OF THE CERVIX
What is a cone biopsy? A cone biopsy is a procedure in which a cone shaped piece of your cervix is removed in order to evaluate and treat cervical dysplasia (abnormal cervical cells). It is also called cervical conization.Why is it performed? You may have a cone biopsy if your pap followed by a colposcopy indicates moderate to severe cervical cell changes. It is also done to remove and treat abnormal tissue. It can also be used to diagnose cervical cancer and to see how extensive the disease is.
How is the tissue removed? A scalpel is used to remove a cone shaped piece of your cervix. The procedure will be done in an operating room with you asleep under general anesthesia.
CERVICAL CERCLAGE
CERVICAL CERCLAGE
Cervical cerclage is a purse-string type suture that keeps your cervix closed to help keep the baby from delivering too early.
DILATION AND CURETTAGE
Dilation and curettage is a procedure that allows your doctor to evaluate and sometimes treat the lining of your uterus (endometrium). Dilation and curettage is done using instruments that gently scrape and remove the endometrial lining.
Dilation and curettage is a procedure done to scrape and collect tissue inside the uterus and/or endometrium, which is the lining inside the uterus. Dilation is the widening of the cervix which allows instruments to pass into the uterus, while curettage is the scraping of the uterine walls. This procedure is performed to remove tissue after a miscarriage, diagnose uterine cancer or other conditions, or treat heavy bleeding. It is performed under general or local anesthesia. A speculum is inserted into the vagina to hold it open, while a dilator opens the cervix. A curette is then inserted to gently scrape the tissue, which is then analyzed by a pathologist.
HYSTERECTOMY
Hysterectomy is the surgical removal of the uterus. The procedure is done either through the abdomen (through a traditional or laparoscopic approach) or through the vagina. A hysterectomy can remove the body of the uterus (supracervical) or body and cervix (total). One may leave or remove her tubes and ovaries depending on reasons for hysterectomy and one’s age. Hysterectomies are typically performed to treat heavy vaginal bleeding, uterine fibroids, pelvic pain, cervical or ovarian cancer, endometriosis and tumors. The surgery usually requires a 1 to 3 day hospital stay and full recovery is expected in six to eight weeks.
Hysterectomy may be a medically necessary in cases such as:
Invasive cancer of the uterus, cervix, vagina, fallopian tubes, and/or ovaries
Severe infection of tubes, ovaries, and uterus
Heavy, irregular vaginal bleeding
Serious complications during childbirth, such as a rupture of the uterus
Pelvic pain relieved by other treatments or sever endometriosis
Pelvic prolapse
For other conditions, it is optimal to evaluate all options before resorting to major surgery.
HYSTERECTOMY SURGICAL OPTIONS
a) Vaginal Hysterectomy describes a surgical procedure in which the uterus is removed through the vagina. One or both ovaries and fallopian tubes may be removed during the procedure, as well. This surgical approach avoids visible scarring and typically allows for a quicker recovery, as well as less postoperative pain and complications as compared with other types of hysterectomy. Risks associated with the vaginal approach include a slight but serious risk of shortening or damaging the vagina.
b) Laparoscopic-Assisted Vaginal Hysterectomy or Supracervical Hysterectomy employs video technology to provide the surgeon with greater visibility when removing the uterus through the vagina. The laparoscopic-assisted approach entails three small external incisions: one in the navel, through which the laparoscope (small video camera) is inserted, and two others in the lower abdomen for the use of surgical instruments. This procedure may be preferred because of the rapid healing time, a less noticeable scar, and less pain, although actual surgery time is longer than the abdominal approach. Because of the longer time in the operation room and the use of extra electronic equipment, this procedure is also costlier than others. Risks associated with the laparoscopic-assisted vaginal approach include a slight risk of bladder injury and urinary tract infection.
c) Abdominal Hysterectomy is fairly standard and remains the most common approach for removing the uterus and other reproductive organs. When performing an abdominal hysterectomy, surgeons can either use a vertical incision or a "bikini cut" incision depending on the scope of the surgery. The vertical incision cuts vertically from the navel to the pubic hair line, while the bikini cut is a horizontal incision made directly above the pubic hairline. The abdominal hysterectomy approach results in a longer recovery period and more noticeable external scarring but requires less specialty surgical skill and may be less costly and more widely available than other approaches.
Sub urethral Sling Procedures: The most common and most popular surgery for stress incontinence is the sling procedure. Today, most of these procedures are being called by the names TVT or TOT. In this operation a narrow strip of material is used either from: cadaveric tissue (from a cadaver), autologous tissue (from your own body), or soft mesh (synthetic material). It is applied under the urethra to provide a hammock of support and improve urethral closure. The operation is minimally invasive and patients recuperate very quickly. For many years it was thought that biologic materials, the patient’s own fascia or cadaveric fascia, would create better more sustainable outcomes. We have found however that synthetic meshes have both the ease of use with no need for harvest as well as superior long term results.
Retropubic Colposuspension: Another option is abdominal surgery in which the vaginal tissues or periurethral tissues are affixed to the pubic bone. The long-term results are good but the surgery requires longer recuperation time and is generally only used when other abdominal surgeries are also required. This procedure can also be performed laparoscopically however long term results are not as good as with the open procedure.
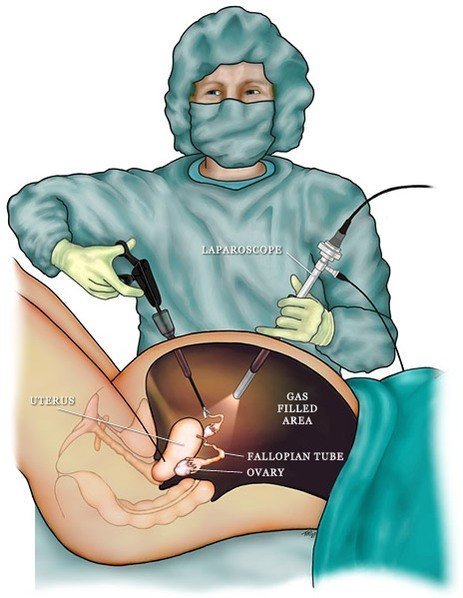
LAPAROSCOPY
Laparoscopy may be used to evaluate and or treat concerns in your abdomen and pelvis. Laparoscopy may used for gynecological concerns as well as infertility concerns. Laparoscopy may be used to perform a hysterectomy. Most of the time laparoscopy is considered same day and you may be able to go home the day of your surgery.
Laparoscopy is a surgery that uses a thin telescope inserted through small incisions in your belly to evaluate and possibly treat the organs in your abdomen and pelvis. Commonly we are able to do laparoscopy instead of Laparotomy (large abdominal incision), which allows a shorter hospital stay and faster recovery. Laparoscopy can used to evaluate and treat problems such as cysts, adhesions, tubal pregnancies, fibroids, infertility concerns, and infection. Laparoscopy can also be used to biopsy tissue and organs inside your abdomen and pelvis to aid in the evaluation of your health concerns.
Laparoscopy is used in Gynecology to:
1. Evaluate for conditions, such as endometriosis, tubal pregnancy, and pelvic infections. 2. Evaluate pain and infertility concerns. 3. Remove tumors and abnormal growths, such as cysts and cancer. 4. Do tubal ligation. 5. Remove uterus, tubes, ovaries and appendix. 6. Biopsy areas of concern.
PELVIC SUPPORT SURGERY
Pelvic floor surgery is used to support your vaginal walls from falling out. This surgery addresses prolapse of the uterus (uterine prolapsed), bladder (cystocele) and rectum (rectocele). This surgery may be done in conjunction with hysterectomy and incontinence surgery.
For information about Bladder and Pelvic Floor Surgery see: Pelvic Prolapse
TUBAL LIGATION
Tubal ligation is the blocking of the tubes in order to prevent the egg from traveling down into the uterus after ovulation, thus preventing conception. This is considered a permanent and non-reversible form of birth control. The failure rate is less than 1%. Tubal ligation may be done through a traditional open incision (mini-laparotomy), or through small incisions (laparoscopy).
Vestibulectomy
Vestibulodynia is pain at the entrance of the vagina (vestibule). Pain may also occur in other parts of the vulva (external genital area), known as vulvodynia. Vestibulodynia is a form of vulvodynia, which causes chronic pain in the vulva, and has no known cause a lot of the time. The pain is exacerbated by pressure from tampons or intercourse. Medications and non medicinal treatments can ease pain.
Your vulva is the outer part of the female reproductive system and is one of the key areas for sexual response and orgasm. It protects your internal reproductive organs, such as your vagina, uterus, and ovaries. It also protects your urethra, the tube that drains your bladder.
Parts of the vulva:
Clitoris.
Inner lips (labia minora).
Outer lips (labia majora).
Vestibule or opening of your vagina.
There are two types of vulvodynia:
What is acquired vestibulodynia?
Vestibulodynia may be noted during:
Pelvic exam.
Prolonged sitting.
Sexual intercourse.
Tight-fitting clothing.
Vaginal penetration with a finger, penis, tampon, or sex toy.
Congenital provoked vestibulodynia: Vestibular pain that one is born with and is noted at the very first attempt of any type of vaginal penetration, such as your first-time having sex or inserting a tampon.
Acquired provoked vestibulodynia: Vestibular pain occurs days, months or years after you’ve experienced pain-free vaginal penetration. This is a condition that develops over time.
As many as 1 in 4 women will experience a type of vulvodynia or unexplained vulvar pain at some point in their lives. The actual incidence of vulvodynia may be higher as some people may be too embarrassed to talk about the problem with their healthcare providers. Others may not seek care because they think the problem is untreatable and something they must live with.
What causes vestibulodynia?
Experts aren’t sure why certain people experience vestibulodynia. It may be that one is born with oversensitive nerves or increase in number of nerves causing hypersensitivity. Some people experience neuroproliferation (also called neuroproliferative vestibulodynia). Their pudendal nerves are hypersensitive to sensations of light touch (allodynia) and pain (hyperalgesia). Neuroproliferation may be congenital or develop as the result of nerve injuries or irritation (acquired).
Who is at risk for vestibulodynia?
Vestibulodynia is most common among sexually active white and Asian people between the ages of 20 and 40. The condition is also more common among people in menopause who experience vaginal dryness and vaginal atrophy
Can surgery (Vestibulectomy) treat vestibulodynia?
Yes. Well documented studies have shown significant improvement, if not complete resolution of pain at the vaginal opening after vestibulectomy. Dr. Bahnmiller is one of the few surgeons specifically trained in vestibulectomy in Eastern Washington. Some people with provoked vestibulodynia (pain at vaginal opening) who don’t respond to treatments benefit from surgery to remove sensitive skin and tissue. This surgery provides permanent symptom relief in many cases.
Labiaplasty
Labiaplasty is a surgical procedure. Labiaplasty decreases the size of the labia minora (genital lips) so that they are flush with the labia majora (outer part of the female genitalia). Labiaplasty requires removal of part of the labia minor and involves a discussion with your surgeon.
Why have a labiaplasty?
There are a host of reasons females have enlarged labia, including childbirth, aging, sexual activity and genetics. Women choose to have surgery for several reasons. Many women suffer from enlarged labia, have trouble with exercise, hygiene, urinary tract infections, sexual activity and other physical activity. Labia minora frequently get caught in clothe, causing discomfort from daily activity to exercise. Certain clothes, such as yoga pants and swimsuits make many women self-conscious with enlarged labia. Most women state that they feel very self-conscious when becoming romantically involved with their partners. These and other reasons are why women decide to have a labiaplasty.
Labiaplasty procedures
There are two types of labiaplasty. Trim and wedge procedure.
Trim procedure
It is the original technique and is most natural to perform. It is also the most widely used technique used by surgeons. In this procedure, the excess part of labia minora is removed and sutured so that it is symmetrical with the labia majora.
Wedge procedure
In this procedure, a partial thickness wedge is removed from the thickest part of the labia minora. The submucosa (layer tissue beneath a mucous membrane) must be left intact by removing only a partial thickness. This procedure gives the vagina a natural look after the surgery as well. We prefer this procedure, since it preserve most of the sensation and gives the best results typically.
If you need to schedule consultation for evaluation and possible treatment (vaginoplasty or MonaLisa), or need any of the above mentioned products (Kegel Cones,V-Fit, Uberlube, Vitamin C, V-Magic)
Labioplasty video: https://www.youtube.com/watch?v=6JO-SGlLW9Y
MYOMECTOMY
Myomectomy is a procedure that surgically removes fibroids (non-cancerous tumors of the uterus), and repairs the uterus for women who plan to bear children or want to keep their uterus. Myomectomy can be done abdominally, laparoscopically, or hysteroscopically depending on the size and location of the fibroids.