WOMEN’S HEALTH & GYNECOLOGY
When a woman has a sexual health problem, it can impact many aspects of her life, including her personal relationships and her self-esteem as well as her overall health.
It is estimated that 43% of American women suffer from sexual health issues. One third of all women, regardless of age, have diminished sexual interest. In addition, nearly one fourth of all women do not experience orgasm, while one fifth of women suffer sexual pain disorders.
EXPLORE YOUR CONCERNS
WHAT IS WOMAN'S HEALTHCARE?
Many women do not have access to a gynecologist or don’t come in for routine checkups and screenings, as they should. It’s incredibly important that women not only have access to a gynecologist but that they also follow through with checkups, screenings and more that pertain to their health and wellness. A gynecologist isn’t just there for you once concerns start to occur, they can help you prevent problems and enhance your sexual life.
WHY IS WOMEN’S HEALTH IMPORTANT?
From cervical cancer screening to sexual wellness, there are many health concerns that affect women and can cause serious health complications that can impact your quality of life. Here at Columbia Shores Regenerative Health, we are here to provide the highest quality care to women of all ages who are living in and around Richland, WA and the greater Tri-Cities area. Women can turn to us for a number of reasons, some of which include,
Routine annual checkups, which include Pap smear, pelvic and breast exams
Menstruation (period) issues
HPV screening
Pelvic pain
Sexual health concerns, such as decreased desire, lack of orgasm, and decreased satisfaction
Incontinence and Bladder concerns
Birth control and family planning options
Menopausal treatments
Hormonal therapies, such as bioidentical estrogen, testosterone and progesterone therapy
Ultrasound evaluation
Vaginal pain
Pain with sex
Vaginal rejuvenation
Infertility and difficulties getting pregnant
Postpartum
Cosmetic Gynecology, such as labiaplasty
Vaginal tightening, such as vaginoplasty
Here at Columbia Shores Regenerative Health, Dr. Bahnmiller also provides minimally invasive surgeries including robotic surgery, which can be used to remove gynecological tumors and fibroids, perform hysterectomies, treat endometriosis, and repair uterine prolapse. Laparoscopic gynecological surgery is far less invasive, which means fewer side effects and complications and a faster recovery period.
It’s important for all women to find a gynecologist that they trust. If you want to turn to the gynecological team here at Columbia Shores Regenerative Health, call our Richland, WA, practice today at (509)572-2130.
GYNECOLOGIC CONCERNS AFFECT A WOMAN THROUGHOUT HER ENTIRE LIFE
We are here at Columbia Shores to partner with you from prevention of gynecological problems to the treatment of gynecologic health issues. We provide services for women's health care and women's sexual health, and more. Please view our services and let us know how we can help you.
ANNUAL EXAMS
You may not need a Pap test every year, but if you’re a woman who is 21 or older, you should have a gynecological (pelvic) exam each year as part of your wellness maintenance. During this exam, we can assess your health and screen you for diseases based on your age and risk factors, and help prevent health issues. .
If you typically see your doctor only when you’re sick, this annual exam might be the first point of contact for detecting any abnormalities with your reproductive organs, or other areas of the body. Yearly visits help your physician detect issues, hopefully before they are advanced, and help you avoid serious complications.
Your Annual exam doesn’t just check your reproductive organs, but your overall health as well. If you are developing high blood pressure or diabetes, this annual exam might detect this, so you have an early start on treating it.
But going to the GYN isn’t just to treat potential illnesses. It’s also a time to talk about how to maintain a healthy lifestyle and minimize health risks. If you have questions about contraception, hormone therapy, planning for pregnancy or are interested in genetic screening to determine if you have an increased risk of cancer due to family history, you can talk with your doctor during the exam.
Other topics to discuss during an annual GYN exam may include:
Menopausal concerns
Hormonal concerns
Vaccinations (such as HPV and others)
Depression screening
Concerns about sex
Weight control
Issue with your menstrual period
Urinary incontinence
What to Expect During A GYN Exam?
Much of the annual exam will be familiar—your vital signs will be taken to get your blood pressure, heart rate and temperature. You’ll get weight and height measurements to determine your body mass index. Your doctor will also examine your abdomen and groin area, checking for masses or enlarged lymph nodes. Most doctors will perform a breast exam and a pelvic exam. The pelvic exam consists of examining the external genital area as well as an internal exam of the vagina, cervix, uterus and ovaries.
How is a Pap Test Different from a GYN (Pelvic)Exam?
A Pap test may be done during the GYN pelvic exam. A pap test (also called a Pap smear or cervical cancer screening) is a specific test that looks in your cervix for abnormalities that could include inflammation, infection, precancerous and cancerous cells. During the exam, cells from the cervix are gently removed and are examined under a microscope to check for any problems.
How Often Do I need a Pap Test?
Although you should have a GYN exam every year, the American Congress of Obstetrician and Gynecologist recommends the following schedule for Pap test:
Under the age of 21—no Pap test needed
Age 21-29: A Pap test every three years, as long as the tests remain negative for abnormalities
Age 30-65: A Pap test and HPV testing, every three to five years, as long as both tests remain negative
Over the age of 65: no Pap test is needed, if negative for the past 3.
If you have had your cervix removed from hysterectomy and no history of abnormal paps you no longer need the pap test
HORMONE THERAPY
HORMONES AND YOUR BODY
Hormones are chemical messengers that affect many body processes, such as metabolism, sexual function, reproduction, and mood. You can develop an imbalance due to natural hormonal transitions or certain medical conditions. This can lead to a variety of symptoms such as menstrual irregularities, skin changes, mood changes, sleep disturbances and weight fluctuations.
1. Hormonal Imbalance Menstrual Symptoms
Irregular periods
Heavy menstrual bleeding
Bleeding between periods
Missed periods
2. Hormonal Imbalance Skin and Hair Symptoms
Acne, especially during adolescence, pregnancy,perimenopause, and menopause
Dryer, thinner skin
Rashes and easily irritated skin
Thinning Hair
Slow wound healing
3. Hormonal Imbalance Digestive Symptoms
Bloating
Diarrhea
Constipation
Sex hormones help regulate the gastrointestinal (GI) tract. Estrogen and progesterone in particular may influence IBS (Irritable Bowel Symptoms). GI symptom changes related to the menstrual cycle are common.
4. Hormonal Imbalance Mood Symptoms
When estrogen and testosterone levels drop during perimenopause, so do Serotonin levels.5 Serotonin is a chemical messenger (neurotransmitter) that helps brain and nervous system cells communicate.
Nervousness
Irritability
Anxiety
Sadness
5. Hormonal Imbalance Weight Symptoms
Weight changes are sometimes the result of a hormonal imbalance. For example, hormone changes due to menopause or having too much or too little cortisol, can result in weight gain. Conditions such as hyperthyroidism can lead to weight loss.
6. Hormonal Imbalance Hair Symptoms
Hormones have a big impact on the hair growth cycle and hair thickness. Anything that affects your hormone levels can affect your hair, causing:
Unwanted facial hair, such as hair under your chin, along your jawline, or above your lip
Thinning hair or hair loss
7. Hormonal Imbalance Sleep Symptoms
Trouble falling asleep or staying asleep
Poor sleep due to night sweats and hot flashes
Insomnia
Poor sleep can make it 10 times more likely that you'll develop depression and significantly worsen your mood.
8. Hormonal Imbalance Sex Symptoms
Low sex drive (libido) can be a symptom of a hormonal imbalance.
Endocrine (hormonal) abnormalities are common in people with sexual dysfunction. Several hormones, primarily testosterone, can affect sex drive. Estradiol, testosterone, and progesterone all help modulate sexual desire in females.
9. Hormonal Imbalance Fertility Symptoms
Ovulation depends on the timing of certain hormones, such as gonadotropin-releasing hormone (GnRH), luteinizing hormone (LH), and follicle-stimulating hormone (FSH). Infrequent or absent periods could mean that you're not ovulating.
Tests to Diagnose the Cause of Hormonal Imbalance Symptoms
Hormones can get out of balance due to natural transitions in life, such as puberty, pregnancy, and menopause. Many medical conditions also affect hormones. That's why it's important to see us at Columbia Shores Regenerative Health to help you optimize your hormone health. Your specific symptoms and clinical examination will determine the next steps.
How to Treat Hormonal Imbalance Symptoms
Treatment depends on the specific diagnosis.
At Columbia Shores Regenerative Health we tailor your treatments to you. Our treatments range from hormonal therapies, bioidentical hormones, in office treatments and non-hormonal therapies. We wish to maximize your potential to get the most joy out of your life.
Summary
Symptoms such as unexplained weight changes, menstrual irregularities, and skin problems may be related to hormonal imbalance. Natural changes, such as puberty, pregnancy, and menopause can cause dramatic hormonal changes, as can medical conditions, such as thyroid problems and PCOS.
Hormonal imbalance is treatable, so take the first step to improving your life and book a consultation today.
MENOPAUSE THERAPY
Menopause
At Columbia Shores Regenerative Health we believe that women entering menopause deserve to feel fantastic.
Women seeking hormonal help receive it only 6% of the time. Menopause is a normal part of a woman’s life, but suffering should not be. Our passion at Columbia Shores Regenerative Health is to help assist you with hormones and life’s changes, thus giving you the most fantastic and exciting feelings of being alive.
We go by the science, not the trends.
Our clinical solutions are created specifically for women as they age and address their unique and individual concerns. We customize your care with both traditional medical treatments as well as bioidentical. Each hormone replacement for menopause treatment(safe! safe! safe!) is customized to you. Along with hormonal treatments, we also offer treatments that improve your sex-life (from creams to vaginal rejuvenation). These treatments not only relieve vaginal dryness and painful intercourse but revive your sex life.
These treatments do not end there. They also improve your skin health and beauty as well as improve your bladder function.
Menopausal Therapies Offered:
Bioidentical Hormones
Estrogen
Testosterone
Progesterone
Hormone pellet therapies
Non-hormonal therapies
Insomnia (sleep difficulties)
Sexual concerns
Progesterone therapy
Weight changes
Genetic testing
Breast Exams and Concerns
TESTOSTERONE THERAPY
Testosterone: Regenerate your mind and body!
Testosterone plays an integral role in both men’s and women’s health — from sex drive and muscle mass to skin and hair health.
At Columbia Shores Regenerative Health, Dr. Bahnmiller can help you optimize your Testosterone and improve not only your sex drive, but improve your energy, weight gain and strength.
Testosterone For Women’s Health
From bone and skin health to sex drive, testosterone influences female health just as much as estrogen and progesterone. It’s the preconceived notions about testosterone that lead most women to fear testosterone rather than embrace it. Women are hesitant to supplement with testosterone out of fear of growing facial hair or developing masculine traits.
Women are constantly telling Dr. Bahnmiller that testosterone has significantly changed their life and they wish they would have started it sooner.
Misleading Fears about Testosterone
Becoming masculine, deep voice, more body hair, and buff muscles
At Columbia Shores RH we closely monitor your levels to ensure you do not even come close to such levels
Association between the type of testosterone used in illegal steroids and bioidentical hormone therapy
At Columbia Shores RH we use bioidentical hormones for supplementing. These are not illegal and dangerous steroids.
Misinformation from health care providers who have well intended but potentially misleading opinions about testosterone and hormone therapy
Symptoms of Low Testosterone in Women
Lost libido and sexual desire
Decreased Orgasm
Depression
Fatigue
Muscle weakness
Weight gain
Hair loss
Hair thinning
Slowed collagen production
Aging skin
Benefits of Testosterone Therapy
Improves Skin And Hair
Testosterone improves the quality of your skin and hair.
Your body’s natural collagen production decreases with age, leaving wrinkled, sagging skin in its place. Testosterone therapy improves your collagen production, thus improving your skin’s health, texture and appearance. Testosterone will make your skin look brighter, and younger.
Testosterone helps improve your hair thickness and helps prevent it from falling out, thus maintaining good growth. Testosterone and thyroid hormones complement one another to stimulate hair growth from follicles in the resting phase. Testosterone therapy does not create new hair follicles, it only helps the follicles you have move back into their growth phase, thus thickening the follicles. This is why women who have had laser hair removal note an increase in hair growth once they start taking testosterone, since it makes hairs that were too stubborn to be treated more treatable. The hairs are not regrowth of effectively treated hairs.
Boosts Your Energy and Mood
Testosterone helps boost your energy by improving your blood count and improving muscle mass.
Balancing your testosterone levels with bioidentical hormone therapy helps lift the veil of brain fog, fatigue and depression. By boosting energy, moods and metabolism testosterone helps you embrace life once again.
The Role of Testosterone in Menopause
Testosterone Peaks in our 20s and then declines 1% a year thereafter. The greatest impact is noticed at menopause when the greatest change in a woman’s hormones occurs.
The years before menopause (perimenopause) testosterone can boost energy stamina, fat burning and improve skin health and sex drive. Dr. Bahnmiller is able to customize your testosterone and hormone therapy to deliver benefits that optimize your well-being and sex life before and into your menopausal years.
Testosterone, Glucose Control and Weight Loss
Typical American eating habits keep our blood sugar levels elevated, thus keeping our insulin increased in our blood system. Our bodies then become more and more insulin resistant leading to difficulty in maintaining our sugars, increasing weight gain and eventually diabetes. Besides diabetes this insulin resistance can increase other health concerns, such as PolyCystic Ovarian Syndrome.
Testosterone can help our body become more insulin sensitive, thus improving sugar control. Testosterone does so by increasing muscle mass, which is more responsive to insulin and also boosts your metabolism. Increase in metabolism helps you maintain blood sugar and a healthy weight. F
Maintain Bone Mass
One of the greatest health risks to women is bone fractures and a leading cause of death for women is hip fracture. Maintaining optimal bone health is essential to our overall health and well being. Weight bearing exercise, vitamin D, calcium, sun exposure estrogen improve your bone health. Testosterone is usually not included in this list, but testosterone has been shown to support bone growth beyond the effects of estrogen alone.
Significant Factor in Sex Drive (Libido)
Almost half of women have a low to absent sex drive. This lack of intimacy significantly impacts their relationship. Testosterone therapy can be the key to resolving this or one of the factors affecting one’s sexual desire.
At Columbia Shores Regenerative Health we can optimize your testosterone therapy and customize a plan to improve your sexual desire and relationships.
Protecting Against Heart Disease
Cardiovascular disease is the leading cause of death in women. Balancing hormones with testosterone therapy can protect themselves against cardiovascular risk factors. Testosterone is a significant factor in decreasing heart disease by improving insulin resistance, maintaining muscle mass, and metabolism, improving energy and activity. Not to mention that increased sexual activity has been shown to improve physical and mental health as well as heart health.
Is Testosterone Not Recommended for Some?
Yes. Women who are pregnant, wishing to become pregnant or have a history of breast (hormone receptor positive), uterine (endometrial) cancer or currently undergoing active cancer treatment should not be on testosterone.
Don’t Let Your Age Change You, Change the Way You Age. Maximize Your Hormones to Maximize You.
WOMEN’S SEXUAL HEALTH
Women’s Sexual Health
Decreased Desire (Hypoactive Sexual Desire Disorder)
Hypoactive sexual desire disorder (HSDD) is a condition in which people lack sexual desire (low libido) or interest, resulting in personal distress or distress in their relationships. It may affect upwards of 50% of women at some point in their lives.
Sexual desire is connected to our self-esteem and the intimacy we have with our partners. Our goal is to provide solutions for women to not only improve sexual desire, but to be able to feel connected to their bodies again.
At Columbia Shores Regenerative Health, we understand the psychological and physical difficulties of HSDD. We are here to support women and are dedicated to creating unique, customized care that helps find solutions that work for you.
Examples of some of our personalized treatments include:
Tailored plasma rejuvenating Sweet Spot Shot
Medications
Sex coaching
Schedule now www.columbiashoresRH.com for a virtual or in person consultation and reignite your sex life.
TREATMENTS
Hormones
Testosterone/bioidentical/estrogen/progesterone
Medications/Compounded Medications
Supplements
Sweet Spot Shot
Mona Lisa Touch
Sex Coaching
Decreased Orgasm/Lack of Orgasm
Orgasmic dysfunction is when someone has difficulty or the inability to reach an orgasm. For some people, reaching a climax can take longer than normal or be unsatisfying.
The way an orgasm feels or how long it takes to have an orgasm can vary widely. When someone has orgasmic dysfunction, climax can take a long time to reach, be unsatisfying, or be unattainable.
Orgasmic dysfunction affects approximately one-third of women. Factors affecting orgasm are physiologic, situational, life-stressors and primary anorgasmia in which someone has never been able to attain an orgasm. Orgasm is not the only goal of sexual intimacy, but may have a significant impact on one’s relationship with themselves or their partner.
Aside from being a board certified Gynecologist (Women’s health expert physician), Dr. Bahnmiller is the only one in the region with extensive sexual health training, which allows him to uncover and treat what may be limiting your sexual relationship and satisfaction. Schedule a live or virtual consultation at www.columbiashoresRH.com and bring the excitement back.
TREATMENTS
Sweet Spot Shot
Dream Cream
Medications
MonaLisa Vaginal Rejuvination
VFit
Dyspareunia/Painful Intercourse
Painful intercourse (dyspareunia) can occur for reasons that range from physical concern, such as menopause, breast cancer and pelvic floor issues, to psychological concerns. Painful intercourse can have a significant impact on a woman’s life, and sometimes may cause a woman to stop having intercourse permanently. Many women have painful intercourse at some point in their lives.
Painful intercourse may occur at any point of a woman’s life, and is more common with aging. Many factors that cause painful intercourse may be resolved and women can enjoy intercourse most, if not all of their lives. Aids such as hormones, lubricants, pelvic floor PT and botox to a multitude of treatments we have the resources that can help eliminate the pain and bring back the pleasure of sex.
Reach out today and schedule a consultation with Dr. Bahnmiller www.columbiashoresRH.com and take back the pleasure of sex.
TREATMENTS
MonaLisa Vaginal Rejuvination
Sweet Spot Shot
Uberlube
Vestibulectomy
VFit
Pelvic Floor Botox
Labial Hypertrophy (Enlarged Labia)
Labial hypertrophy describes the enlargement of the vaginal lips. The Labia Majora are the outer lips of the vulva and the Labia Minora are the inner lips. The Labia Minora are the lips most often enlarged or cause symptoms or discomfort. The labia help cushion the inner vagina and clitoris from friction, impact, and damage and are usually enlarged as a result of genetics or childbirth.
A woman may choose to have a labiaplasty (reduction in size of the lips), due to discomfort from being caught in clothing to self image; especially while wearing tight clothing such as yoga pants. Many women elect to reduce the size of their labia for discomfort and cosmetic reasons. Dr. Bahnmiller has additional training in treatments, such as labiaplasty (cosmetic surgical correction of the labia), laser surgery, and medical treatments to give you the feel and look you desire. Schedule a consultation with Dr. Bahnmiller today at www.columbiashoresRH.com to design a treatment plan for you.
TREATMENTS
Labiaplasty
Vaginoplasty
Testosterone Therapy
Symptoms of low testosterone may be seen as normal signs of aging. Low testosterone levels in women can cause a variety of life altering symptoms, much the same as they do in men. Symptoms of low testosterone include, but are not limited to fatigue, weight gain (especially in the abdomen), difficulty losing or maintaining body weight, decreased sex drive (libido), anxiety, hair loss, decreased strength or workout ability, and brain fog.
We can help restore a balance of your testosterone to restore your vitality using testosterone supplementation that fits you. Our program not only offers bioidentical replacement options, but Dr. Bahnmiller personally sees you and watches you and your levels to ensure the treatment you receive is safe and effective. We offer conveniences from creams, sub-Q injections to pellet therapy, so you can get back to enjoying your life. Schedule a consultation with Dr. Bahnmiller today at www.columbiashoresRH.com to see if testosterone therapy can help get you back to you.
TREATMENTS
Testosterone therapy
Pellet therapy
Menstrual disorders are concerns that affect a woman’s normal menstrual cycle and have an impact on her daily life. Menstrual disorders include:
Painful cramps (dysmenorrhea) during menstruation.
Heavy bleeding (menorrhagia) includes prolonged menstrual periods or excessive bleeding.
Absence of menstruation (amenorrhea).
Infrequent menstruation (oligomenorrhea) refers to menstrual periods that occur more than 35 days apart.
Treatment may include:
Dilation and curettage may help restore your normal cycles.
Endometrial ablation is a surgical option. This should only be considered when you are done childbearing, and you should use a highly effective form of birth control.
Hysterectomy may be the treatment of choice for some women.
MENSTRUAL DISORDERS
Dysmenorrhea (Painful Cramps)
Dysmenorrhea is severe, frequent cramping during menstruation. Pain occurs in the lower abdomen but can spread to the lower back and thighs.
Menorrhagia (Heavy Bleeding) Menorrhagia is the medical term for significantly heavier periods. A rough gauge is changing your pad more than 3-6 times per day. Women should consult their doctor if any of the following occurs:
Soaking through at least one pad or tampon every 1 - 2 hours for several hours
Heavy periods that regularly last 7 or more days
Bleeding between periods or during pregnancy. Spotting or light bleeding between periods is common in girls just starting menstruation and sometimes during ovulation in young adult women, but it is still a good idea to speak with a doctor. Women who experience any post-menopausal bleeding should definitely contact their doctors.
Flow that is longer or heavier than your normal.
Metrorrhagia (Irregular bleeding) Metrorrhagia also called breakthrough bleeding. The bleeding occurs between periods or is unrelated to periods.
DYSMENORRHEA (PAINFUL PERIODS)
Dysmenorrhea is caused by prostaglandins, hormone-like substances that are produced in the uterus and cause the uterine muscle to contract. Prostaglandins also play a role in the heavy bleeding that causes dysmenorrhea.
Dysmenorrhea can be caused by a number of medical conditions.
Endometriosis is a chronic and often progressive disease that develops when the tissue that lines the uterus (endometrium) grows onto other areas, such as the ovaries, bowels, or bladder.
Uterine Fibroids are benign growths that grow in the muscular wall of the uterus. They can cause heavy bleeding during menstruation and cramping pain.
Other Causes. Pelvic inflammatory disease, ovarian cysts, ectopic pregnancy, and the intrauterine device (IUD) contraceptive can also cause dysmenorrhea.
SURGICAL OPTIONS
Women with heavy menstrual bleeding, painful cramps, or both have surgical options available to them. Most procedures eliminate or significantly affect the possibility for childbearing, however.
Endometrial Ablation destroys the entire lining of the uterus (the endometrium). For most women, this procedure stops the monthly menstrual flow. In some women, menstrual flow is not stopped but is significantly reduced.
Endometrial ablation is not appropriate for women who:
Have recently been pregnant
Would like to have children in the future
Have certain gynecologic conditions such as cancer of the uterus, endometrial hyperplasia, uterine infection, or an endometrium that is too thin
Hysterectomy is the surgical removal of the uterus. However, with newer medical and surgical treatments available, hysterectomies are performed less often than in the past. Hysterectomy, unlike drug treatments and less invasive procedures, cures menorrhagia completely, and most women are very satisfied with the procedure. Hysterectomy may or may not be done with or without removal of your ovaries.
MENSTRUAL DISORDERS
Urinary incontinence is the unintentional loss of urine. The severity of urinary incontinence ranges from mild episodes to significant loss of urine.
If urinary incontinence affects your day-to-day activities, don't hesitate to call us. Most cases, simple lifestyle changes or medical treatment can ease your discomfort or stop urinary incontinence.
Types of urinary incontinence include:
Stress incontinence. This is loss of urine when you exert pressure on your bladder by coughing, sneezing, laughing, exercising or lifting something heavy.
Urge incontinence. Urge incontinence is the loss of urine, due to uncontrollable muscle spasm of your bladder.
Overflow incontinence. If you frequently or constantly dribble urine, you may have overflow incontinence, which is an inability to empty your bladder. Sometimes you may feel as if you never completely empty your bladder.
Mixed incontinence. If you experience symptoms of more than one type of urinary incontinence, such as stress incontinence and urge incontinence, you have mixed incontinence.
COMPLICATIONS
Skin problems. Urinary incontinence can lead to rashes, skin infections and sores (skin ulcers) from constantly wet skin.
Urinary tract infections. Incontinence increases your risk of repeated urinary tract infections.
Changes in your activities. Urinary incontinence may keep you from participating in normal activities. You may stop exercising, quit attending social gatherings or even stop venturing away from familiar areas where you know the locations of toilets.
Changes in your work life. Urinary incontinence may negatively affect your work life. Your urge to urinate may cause you to have to get up often during meetings. The problem may disrupt your concentration at work or keep you awake at night, causing fatigue.
Changes in your personal life. Perhaps most distressing is the impact incontinence can have on your personal life. Your family may not understand your behavior or may grow frustrated at your many trips to the toilet. You may avoid sexual intimacy because of embarrassment caused by urine leakage. It's not uncommon to experience anxiety and depression along with incontinence.
WHAT YOU CAN DO
Print Off and Fill out our Voiding Diary PDF
Write down key personal information, including any major stresses or recent life changes.
Bring a list of all medications, vitamins or supplements that you're taking.
Testing
If further information is needed, you may undergo additional testing, including:
Postvoid residual (PVR) measurement. For this procedure, you're asked to urinate (void) into a container that measures urine output. Then your doctor checks the amount of leftover (residual) urine in your bladder using a catheter. A large amount of leftover urine in your bladder may mean that you have an obstruction in your urinary tract or a problem with your bladder nerves or muscles.
Pelvic ultrasound. Ultrasound also may be used to view other parts of your urinary tract or genitals to check for abnormalities.
Stress test. For this test, you're asked to cough vigorously or bear down as your doctor examines you and watches for loss of urine.
Urodynamic testing. These tests measure pressure in your bladder when it's at rest and when it's filling. A doctor or nurse inserts a catheter into your urethra and bladder to fill your bladder with water. Meanwhile, the pressure in your bladder is monitored. This test helps determine what type of incontinence you have.
TREATMENTS
Treatment depends on the type of incontinence, the severity of your problem and the underlying cause. A combination of treatments may be needed.
Initially we will suggest the least invasive treatments first. We usually begin with behavioral techniques and physical therapy first and add other treatments as necessary.
At Columbia Shores Regenerative Health we are able to treat your incontinence from behavioral techniques, pelvic floor exercises, to surgery and bladder Botox.
BEHAVIORAL TECHNIQUES
Behavioral techniques and lifestyle changes work well for certain types of urinary incontinence. They may be the only treatment you need.
Bladder training. We may recommend bladder training. This type of therapy may used alone or in combination with other types of therapy. In bladder training you begin with a frequency of urination that you are able to maintain. Once you able to keep the initial voiding schedule we have you then add 15 minutes between each void until you are able to void on schedule every 2 to 4 hours.
Fluid and diet management. In some cases, you can simply modify your daily habits to regain control of your bladder. You may need to cut back on or avoid alcohol, caffeine or acidic foods. Reducing liquid consumption, losing weight or increasing physical activity are other lifestyle changes that can help.
PHYSICAL THERAPY
Pelvic floor muscle exercises. These exercises strengthen your urinary sphincter and pelvic floor muscles to help control your bladder. Pelvic floor exercises or physical therapy has a significant impact on improving both stress urinary incontinence and urge incontinence.
Kegal Cones. These are a good adjunct to pelvic floor exercises. Initially you insert the largest cone vaginally and hold while standing upright for 10 minutes in the am and 10 minutes in the pm. Once you can keep the cone in for these durations, 2x a day for 2 weeks then you move to the next size smaller and heavier until you get to the last cone. Once at the last cone you continue on this regiment. These cones may be ordered from online stores such as Amazon.
MEDICATIONS
Often, medications are used in conjunction with behavioral techniques. Drugs commonly used to treat incontinence include:
Anticholinergics. These prescription medications calm an overactive bladder, so they may be helpful for urge incontinence. Possible side effects of these medications include dry mouth, constipation, blurred vision and flushing.
Estrogen. Estrogen may be taken orally in a systemic form or topical to help with both vaginal and bladder health.
Imipramine. Imipramine (Tofranil) is a tricyclic antidepressant that may be used to treat mixed (stress and urge) incontinence.
MEDICAL DEVICES
Several medical devices are available to help treat incontinence. They're designed specifically for women and include:
Pessary (PES-uh-re). Your doctor may prescribe a pessary — a stiff ring that you insert into your vagina and wear all day. The device helps hold up your bladder, which lies near the vagina, to prevent urine leakage. You need to regularly remove the device to clean it. You may benefit from a pessary if you have incontinence due to a dropped (prolapsed) bladder or uterus.
SURGERY
If other treatments aren't working, several surgical procedures have been developed to fix problems that cause urinary incontinence.
Sling procedures. A sling procedure uses a synthetic material or mesh to create a pelvic sling or hammock around your bladder neck and urethra. The sling helps keep the urethra closed, especially when you cough or sneeze.
Bladder neck suspension. This procedure is designed to provide support to your urethra at the level of the neck of your bladder. It involves an abdominal incision, so it's done using general or spinal anesthesia.
URINARY INCONTENENCE
COSMETIC GYNECOLOGY
-
Labiaplasty is a surgical procedure. Labiaplasty decreases the size of the labia minora (genital lips) so that they are flush with the labia majora (outer part of the female genitalia). Labiaplasty requires removal of part of the labia minor and involves a discussion with your Dr. Bahnmiller to plan your wishes.
-
If you have discomfort from your labia being entrapped in clothing, discomfort during exercise or wishing improved cosmetic appearance of your labia, especially while wearing swimwear or yoga pants you are a candidate.
-
Vaginoplasty is a surgical procedure that tightens the vaginal opening, and helps build pelvic floor support. Vaginalplasty is great to improve vaginal laxity and help improve pelvic floor and bladder support. This can be done by itself or in conjunction with other surgeries, such as labiaplasty.
-
Dr. Bahnmiller offers a wealth of experience in female sexual health, and dysfunction. Now providing The Sweet Spot Shot, helping women find their sexual confidence through non-invasive Vaginal Regeneration.
The Sweet Spot Shot is an all-natural, non-surgical procedure that can regenerate and revitalize vaginal and clitoral function, giving you dramatically improved sensitivity, lubrication, bladder support and significantly enhance your sex life.
Many women lose urine while coughing, laughing, sneezing or exercising. It can be an embarrassing and frustrating problem. Because The Sweet Spot Shot offers bladder support regenerative capabilities. There is help available without the need for invasive surgery.
The entire process has minimal pain, takes less than 30 minutes and in some patients, the results are immediate. The Sweet Spot Shot procedure for incontinence and sensitivity is a revolutionary approach to restoring bladder function and the loss of sensations patients may have.
-
The Life Changing Vaginal Regenerative Treatment for the Prevention and Rejuvenation of your Vaginal Health.
The MonaLisa Touch® is an office based treatment for vaginal changes, such as decreased lubrication and sensation, loss of bladder control, birth trauma and menopausal changes. This unique Vaginal Regeneration was specifically created for the vaginal and bladder mucosa as well as the vulva (Labia minora, labia majora, vestibule and clitoris). The MonaLisa Touch® prevents tissue/nerve loss and resolves estrogen/testosterone drops in the vaginal tissue (typically occurring during menopause or after child birth) by gently acting on tissue of the vaginal mucosa which reactivates the production of new estrogen receptors, youthful healing genes, and collagen, and reestablishes the functionality of the treated area, restoring the proper trophic balance to the mucous membranes of the vaginal and bladder.
Come in for a MonaLisa Touch® treatment at Columbia Shores Regenerative Health and restore your bladder and sex life today!
(509)572-2130
The MonaLisa Touch® treats:
Post menopausal issues
Post Vaginal Birth Trauma
Loss of sensation during sex
Vaginal laxity
Loss of Vaginal sensation
Vaginal dryness
Urinary urge and stress incontinence
Itching and burning
Vaginal tears
Loss of elasticity and tone
Painful intercourse
-
Clitoral Hood Release, is a cosmetic gynecological procedure which may improve clitoral sensation and orgasm. The procedure involves opening up the clitoral hood and exposing the clitoris in order to allow improved sensation of the clitoris, thus improving orgasm.
“I have had thinning hair as long as I can remember, and I come from a long line of family members with hair loss. I heard about the process of putting your own blood back into your head for hair growth from my hair dresser, who has seen results herself, so I decided to give it a try. I figured I had nothing to lose. I have competed three treatments, and notice that the results are getting better over time. A few things I did wish that I would have known before the treatments were done are: Drink a lot of water before procedure. She will draw 60cc of blood, and that seems like a LOT when you aren’t hydrated well. Your head will be numbed first, and ice is applied, but the treatments still don’t feel very good when you feel the blood being injected. It’s a small price to pay for having my hair back though! I also wish I would have brought a hat with me to wear out of the office my first treatment. Aside from that, I am very satisfied with my results, and I have recommended this treatment to many of my family members, who have also had it done.”
INFERTILITY
Infertility is a common condition affecting approximately 12% of couples at some point in their reproductive lives. A healthy fertile couple generally has about a 20 percent chance of conceiving during any one month, and up to 90% chance of conceiving within a year of unprotected intercourse. Infertility is defined as the inability to conceive after 12 months of unprotected intercourse. As we age our risk of infertility increases; therefore, women over the age of 35 may be evaluated and treated for infertility after 6 months of unprotected intercourse.
Infertility may occur if you have never had a pregnancy (primary infertility), or if you have had children (secondary infertility). Both forms of infertility require individualized evaluation and treatment, which we will be happy to assist you with. Some of the evaluation and treatment options you may need include:
EVALUATION OPTIONS
1. Evaluation of ovulation.
a. Physical exam
i. Physical exam is performed in office at initiation of treatment to ensure there are no physical limitations of conceiving. If there any concerns, these will be discussed with you.
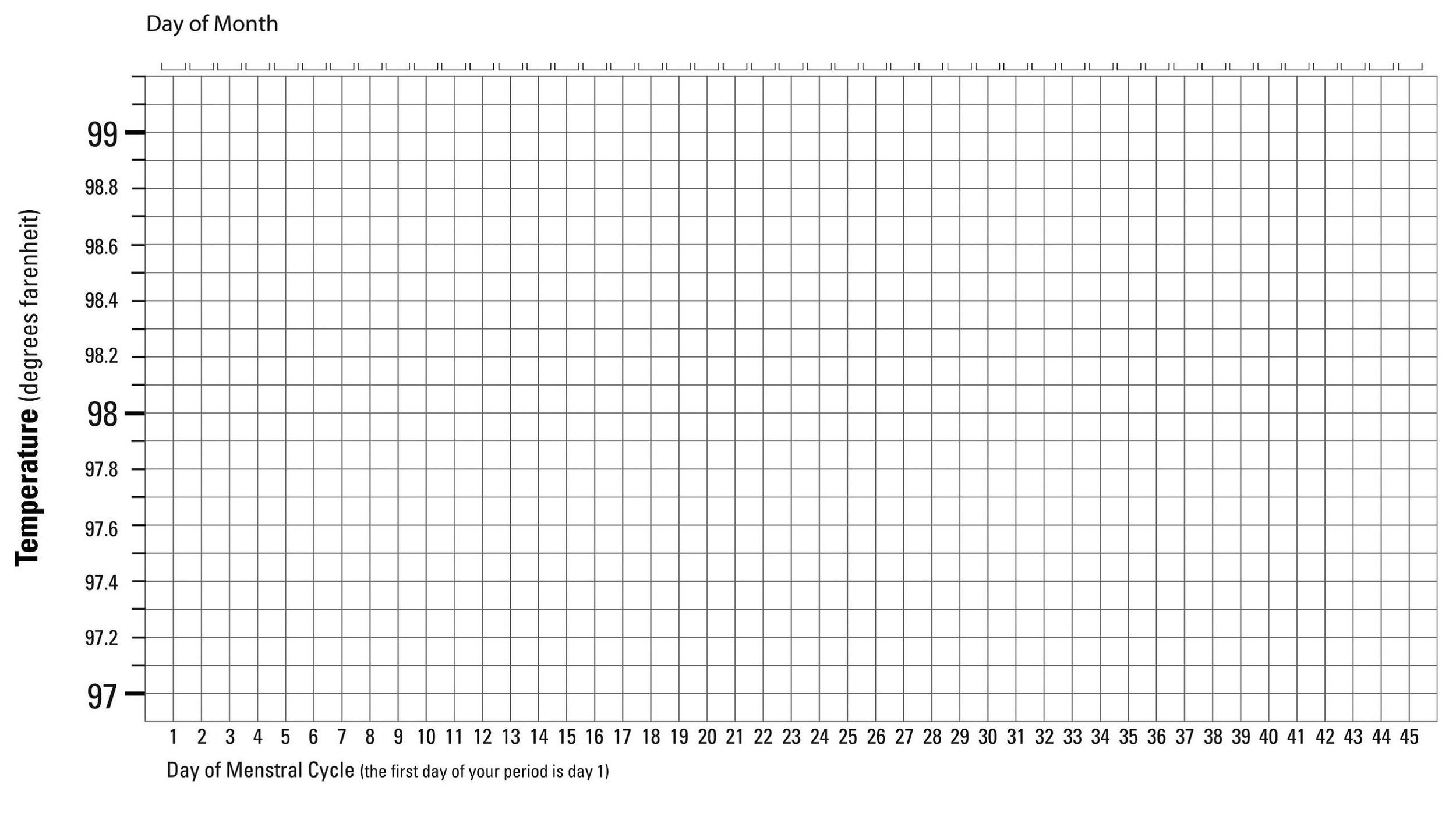
b. Body changes, due to hormones and ovulation.
i. Cervical mucus changes and temperature changes are important signs of ovulation to monitor for.
c. Cycle evaluation
i. Monitoring your menstrual cycle can show optimal days to attempt conception and help point out possible concerns of conceiving. ii. Menstrual diary (aid to monitoring both menstrual changes and cervical mucus changes)
d. LH surge
i. Using an ovulation predictor can help with timing of intercourse or insemination. The LH kit changes color (usually blue) just prior to ovulation, usually 24 to 36 hours before (clear blue and easy is an example of an ovulation kit).
e. Blood laboratory testing
i. Can help evaluate ovarian and endocrine function and/or problems.
f. Ultrasound evaluation of ovulation
i. Can be used to monitor healthy follicle development and timing of treatments.
2.Evaluation of male effect on infertility. (Occurs in one half of couples)
a. Semen analysis. If instructed to do so please follow these instruction.
i. Obtain a sterile specimen cup from our office or the lab, and call the main TriCities Lab on Grandridge in Kennewick to schedule a time to drop off specimen. 7131 Grandridge Blvd (509) 736-0100
ii. Provide a sample by ejaculating into the cup. Don’t use a condom for collection since some of the lubricants or condoms contain spermicidal in them and may effect the results.
iii. Keep close to body temperature by keeping close to your body.
iv. Present specimen to lab within an hour of producing.
3.Evaluation of female physical means of infertility.
a. Physical exam
b. Hysterosalpingogram (HSG) A (HSG) is a special kind of x-ray. An HSG is an outpatient procedure, which takes no longer than a half hour. It involves placing an iodine-based dye through the cervix and taking x-rays to help evaluate the shape of the uterus and whether or not the fallopian tubes are open or blocked. If necessary we will give you an order to have completed at the radiology center. You will need to call and schedule the procedure and afterwards we will review to determine if any further testing/treatment should be done.
c. Laparoscopy. Due to your history and physical exam, a laparoscopy may be necessary to evaluate and treat concerns affecting your ability to become pregnant. If necessary follow the instructions under Laparoscopy in our Hospital Surgeries of our Procedures section of our web site.
d. Ultrasound.
TREATMENT OPTIONS
1. Timing and frequency of intercourse
a. Optimal timing of intercourse is the 2 days prior to ovulation and the 2 days following.
b. Frequency of intercourse increases your chances of becoming pregnant. The week of ovulation, it is optimal to have intercourse 4 times. 3 times is ok and 2 or fewer times during that week make it difficult to conceive. It is of no benefit to abstain before trying or to have a break between attempts.
2. Ovulation monitoring and induction.
a. If we cannot clearly determine if you are ovulating from home testing we may proceed with evaluation in office, by lab testing, physical exam and ultrasound.
b. Ovulation may need to be augmented with cycling and stimulation of ovulation. Medications used include
i. Clomid ii. Femara iii. Glucophage
3. Intrauterine insemination (IUI).
4. Fertility center treatments. If your care requires more intense monitoring and treatment we may refer you to a Fertility center. These include.
a. IVF/endocrine centers
b. Napro fertility centers
FERTILITY AIDS
a. Basal Body Temperature Chart
b. Ovulation calculator - http://www.marchofdimes.com/pregnancy/ovulation-calendar.aspx?gclid=CNGFrpuOmL0CFYdFMgodEw8AZg#
c. IUI
d. Clomid/Femara. These medications are oral medications that help increase the likelihood of ovulating. If you are prescribed these medications we will have you take them once a day for days 3-7 or 5-9 after the first day of your menses. After taking these medications we will monitor your ovulation and determine your optimal time of attempts of conception. Concerns with clomid use are increased risk of multiples, such as twins and triplets and increased risk of ovarian cancer with prolonged use of. These medications may give you menopausal symptoms, such as hot flushes, vaginal dryness and mood changes.
BASAL BODY TEMPERATURE CHART
IUI (Intrauterine Insemination)
Intrauterine insemination (IUI) is a common treatment for infertility. It can be used in cases where the male has a low sperm count, the cause of infertility is unknown, or when the woman is not ovulating regularly. It may be used with or without medications that help the woman ovulate.
Timing of the insemination to coincide with ovulation is critical. In order to ensure this occurs, timing of ovulation is monitored by urinary hormone tracking methods or sonogram. Urinary LH ovulation predictor kits indicate that ovulation will occur within a 24 to 36 hour window. The urinary tracking method is performed at home, generally in the morning. When the test is “positive”, call us immediately, so we can schedule your insemination, since it should be done within 24-36 hours of a positive test.
Another method used to time ovulation is sonography. The development of the follicle and impending release of the egg can be timed by serial ultrasounds performed in the office. We may give you an injection of HCG to further assist in the release of the egg.
Once we schedule your Intrauterine insemination, please follow the steps below.
INSEMINATION STEPS
Pick up sterile cup from the office 2. Collect semen into sterile cup by masturbation 3. Bring specimen to office in sterile cup. Be sure to bring in within an hour of producing and keep close to body temperature by keeping close to body. 4. Specimen is left at office. Be sure to sign the consents allowing us to use your sperm for the insemination. 5. Sperm is prepped in special media. This clears out abnormal sperm and allows the sperm to penetrate the egg. This procedure takes about an hour. 6. Woman signs consent for insemination. 7. The “washed” specimen is placed with a special catheter into the woman’s uterine cavity in order to improve the number of sperm available to reach the egg by bypassing the vagina and cervix. 8. Since IUI relies on the natural ability of sperm to fertilize an egg within the reproductive tract, the sperm function of the male must be reasonable and the fallopian tube(s) must be healthy and functional. 9. After the insemination, the woman lies for about 20 minutes and then may return to her normal function.
You should begin a prenatal vitamin with at least 800mcg of folic acid before you begin fertility treatment.
If you do not have a period following insemination and have a positive pregnancy test call to schedule your prenatal care. If you have a period following insemination, call and we will discuss your further treatment options. (509) 572-2130
How IUI Works